As the U.S. senior population increasingly struggles with behavioral health conditions, more providers are starting to invest in solutions.
Elara Caring and Oak Street Health (NYSE: OSH) are two such providers looking to help treat seniors’ behavioral health needs through an integrated model of care.
Texas-based Elara Caring is a home health, hospice, personal care, palliative care and behavioral health provider. The home health-focused operator has a 16-state footprint. It is payer agnostic and works with Medicare, Medicaid and commercial payers.
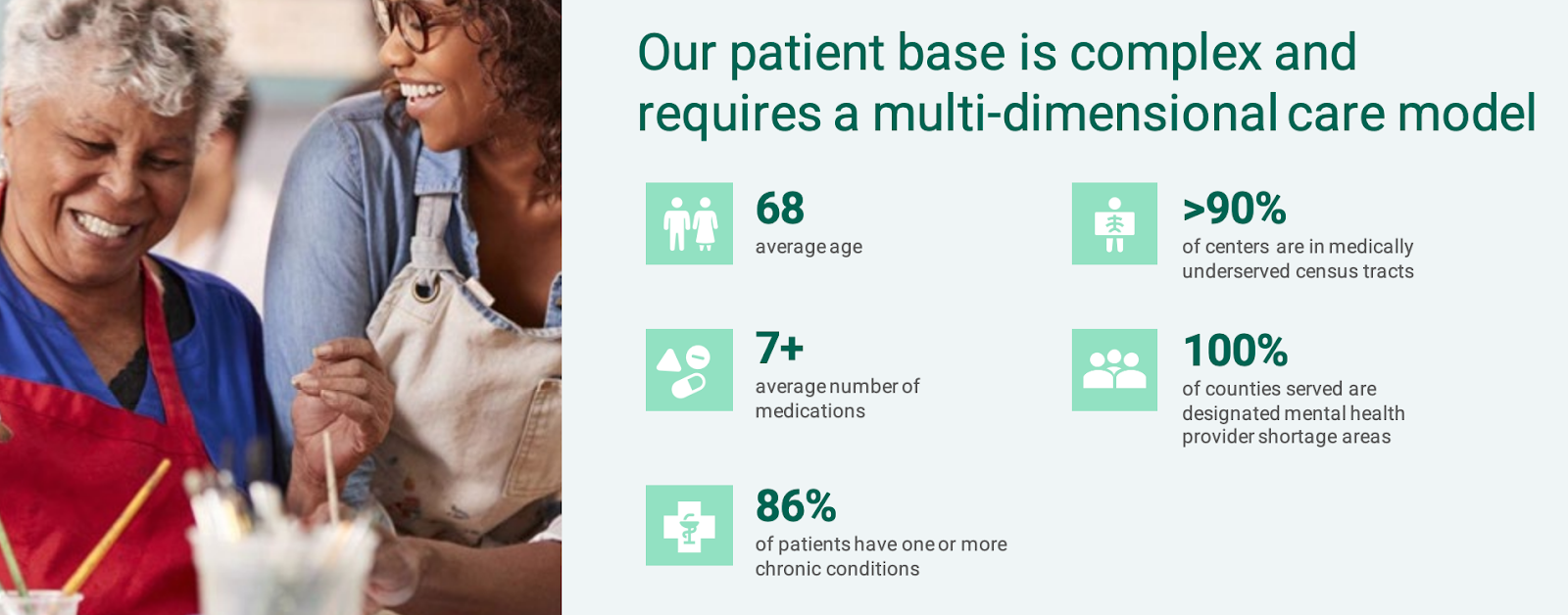
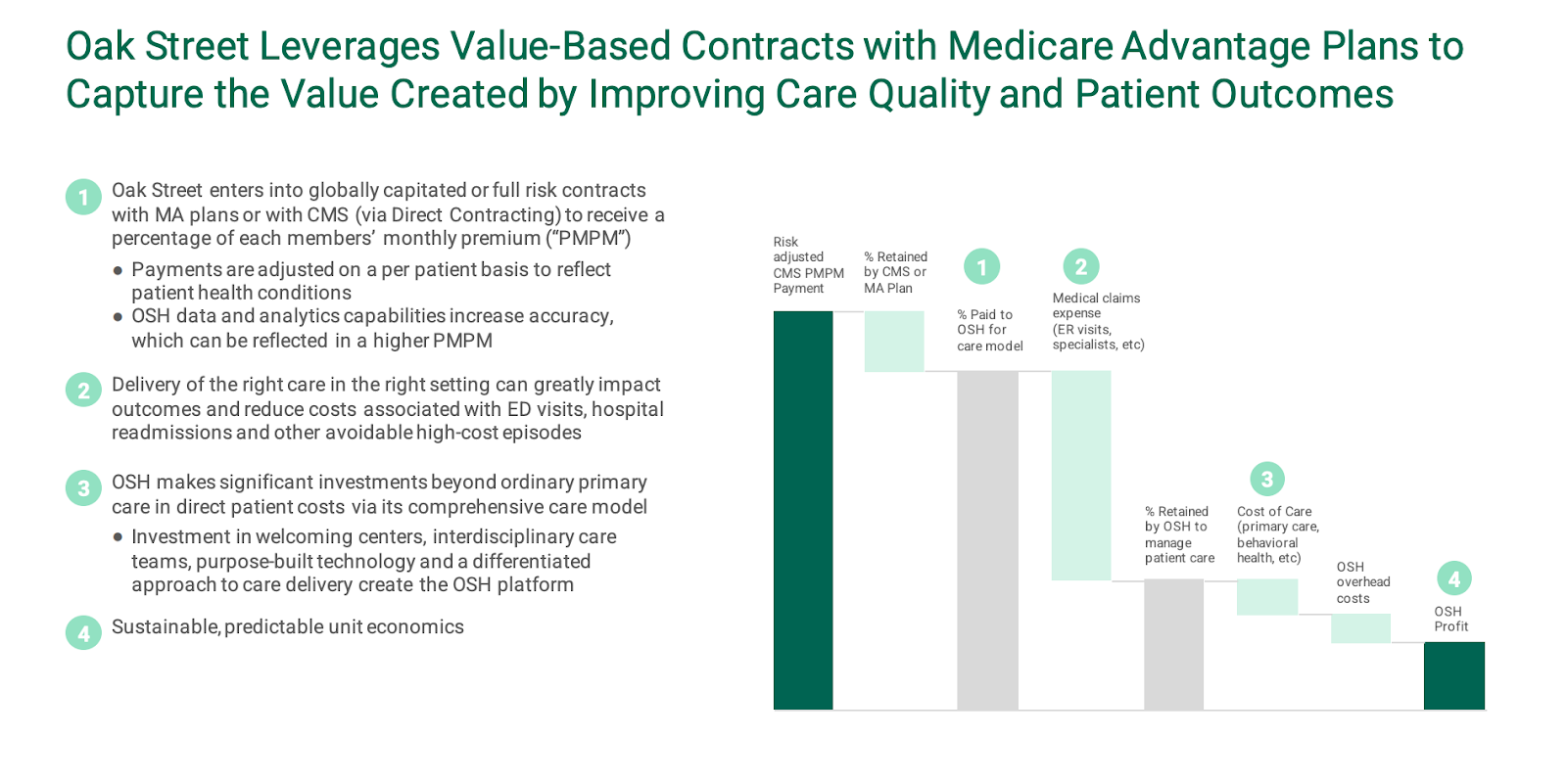
Meanwhile, Oak Street Health is a network of value-based primary care facilities that serve adults on Medicare. As of November, the Chicago-based provider had 161 centers in 21 states, with over 145,000 at-risk patients receiving its care.
“It’s hard to separate the head from the rest of the body,” Katherine Suberlak, vice president of clinical services at Oak Street Health, said Thursday during Aging Media Network’s Continuum conference.
More than a quarter of adults ages 65 to 74 report feelings of anxiety or depression, according to a Kaiser Family Foundation report. Additionally, the rate of deaths from drug overdoses among people 65 and older have tripled over the last two decades, according to recent CDC data.
Those and other statistics have made investing in behavioral health table stakes for senior care providers.
Collaborative care for seniors makes sense for a number of reasons, according to Suberlak, whose organization brought in $546 million in revenue during 2022’s third quarter.
Seniors often have an established relationship with their primary care provider. At the same time, many seniors in underserved communities don’t have access to behavioral health services. If these providers could help coordinate care for seniors, it could expand access, Suberlak explained.
Oak Street employs roughly 5,900 individuals, with about 600 being primary care providers.
“It’s the right thing for the patient, clinically,” Suberlak said.
Additionally, integrated care models could help save money downstream. Mental illness directly impacts a patient’s ability to engage in health care, come to appointments, keep appointments and take their medications, Suberlak said. Ultimately, an untreated mental illness could lead to higher health care utilization.
“It’s very helpful to our care teams to have the added specialty there,” she continued. “And then lastly, we see the outcomes, that it impacts our total cost of care when we include behavioral health as a service to our patients.”

Integration in practice
Oak Street is also working to fully integrate behavioral health into the continuum of care. It uses a collaborative care model and an evidence-based approach to universally screen all patients for both mental health and substance use disorder conditions.
Of the counties the company serves, 100% are designated as mental health provider shortage areas.
Nearly half – 42% – of Oak Street’s patients are dually eligible for both Medicare and Medicaid, according to the company. On average, Oak Street’s patients have seven or more chronic conditions.
“From there, there’s proactive enrollment with a qualified mental health professional that is on site and an embedded part of the care team, assisting both with diagnostics and treatment,” Suberlak said. “Then we have a virtual team of over 10 psychiatric providers that cover the network. So when escalation is necessary, they can help build out that triad around the patient of the primary care provider, psychiatrist and the qualified mental health professional.”
Oak Street has seen positive results in its integrated model. In fact, 73% of patients that enroll in its collaborative care model report experiencing a sustained reduction in depression at 6 months post treatment, Suberlak noted.
“So they are not only feeling better, but are then able to better manage their other illnesses, which we know will impact the other piece,” Suberlak said.
As the need for behavioral health care in the senior population grows, Oak Street Health is looking to scale. Specifically, the provider is aiming to integrate behavioral health services from the get-go when opening a new center.
In total, Oak Street invested nearly $350 million in its care centers and their surrounding communities in 2021.
“So rather than integrating after an opening, integrating from the start,” she said. “A celebration we had just a week ago was opening our centers in Colorado. … We were able to hire, train and onboard our behavioral specialists before we opened, so then they can be part of the team from the start. So our focus will continue to be to have it be part of the full care model.”
Elara Caring similarly uses an integrated approach to care. The in-home care provider looks at both the physical and behavioral health of a patient together. It currently does 100,000 in-home visits for patients with serious mental illness or substance use disorder.
Recently, it developed a program, dubbed Embrace, aimed at helping its members who have experienced loss. That could be loss of a loved one, their independence, their home or another kind of loss. Patients can access the program at home, which could be a skilled nursing facility (SNF), senior living facility or private residence.
“Roughly 50% of individuals going into senior living or a SNF have elevated anxiety or depression,” Joe Cramer, president of hospice and behavioral health at Elara Caring, said at Continuum. “So our nurses are really trained on supporting their behavioral health diagnosis.”

Elara, in particular, reflects how more senior care providers are investing in behavioral health services. Traditionally, home health and hospice companies like the PE-backed Elara have not had dedicated behavioral health service lines.
“Typically, it’s let’s focus on the medical first and then get to the behavioral,” Cramer said. “With Elara Caring, we focus on the behavioral with the medical conditions there. So really looking at what’s causing the anxiety, depression, if they have that, and what kind of loss they’re dealing with to really support them.”
With the Embrace program, Elara Caring reports a 78% reduction or stabilization of a patient’s anxiety or depression.
Elara Caring is looking to expand its behavioral health services into every state it works in. It’s looking to do this through more partnerships with ACO Medicare groups and Medicare Advantage plans.
Additionally, it is looking to expand through more training programs, Cramer said.
